Infectious diseases are caused by outside or internal organisms including viruses, bacteria, fungi and parasites9. Infectious diseases can be spread in a variety of ways including contaminated water or food, bodily fluids, and a disturbance in the internal balance of organisms.9
HIV
HIV is an abbreviation for human immunodeficiency virus. While some viruses can be fought off by the immune system or cured by various medicines, HIV is not one of these viruses. While HIV is treatable there is no cure9.
HIV functions by attacking CD4 cells, also known as “T cells”. These cells help a person’s body fight off infections. If left untreated HIV can lead to a suppression of the body’s immune system enabling other infections to infect the body signaling the transition from HIV to AIDS9.
While there is no cure as of yet, the current treatment protocol, antiretroviral therapy also known as ART, can help reduce the viral load in a patient’s body lowering the risk of transmission and allowing someone to live a full life9.
TasP: Treatment as Prevention
Antiretroviral therapy, or art for short, can be used to treat HIV, but also as a prevention option8. The key to this treatment is that Art needs to be taken regularly, and viral load levels need to be checked regularly. Once viral load is undetectable then it is untransmutable according to new research8.
- Undetectable is also known as virally suppressed8
- Viral suppression is when a patient has less than 200 copies of HIV per milliliter of blood
- Treatment as prevention is also known as U=U12
- Undetectable = Untransmittable
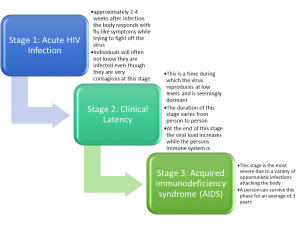
Stages of HIV infection1
Facts on HIV
National
The CDC estimates 1.1 million people are living with HIV in the United States1
1 in 7 are unaware of their HIV status11
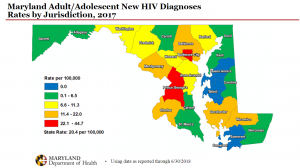
State
At the end of 2016, there were 30,430 adults and adolescents living with HIV in Maryland10
Baltimore-Columbia-Towson Metropolitan Statistical Area (MSA) had the 14th highest estimated HIV diagnosis rate (per 100,000) of any major metropolitan area in the U.S population6
CDC estimates that 14.0% of people living with HIV in Maryland were undiagnosed as of 20155
Over 6,000 people died from an HIV-related illness in 201411
Map sourced from 9.17.18 Maryland PrEP summit
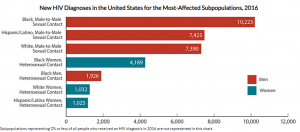
At Risk Populations
HIV disproportionally affects those who are below the poverty line and those who are homeless4
If trends continue 1 in 6 MSM (Men who have sex with men) in the United States will be HIV positive12
Nearly half of new cases in 2016 were Black or Latino MSM 12
52% of new cases occurred in the Southern region of the United States12
Heterosexual black women represent the largest group of new infections among women11
PrEP
Pre-exposure prophylaxis (PrEP) is a prescription medicine that when taken daily can reduce the risk of someone contracting HIV.2
PeP
PEP (post-exposure prophylaxis) is a prescription of antiretroviral therapy (ART) given to someone who has been exposed or was at risk of being exposed to HIV.3
ART
ART, antiretroviral therapy, is the current way that health care providers treat HIV. ART helps reduce viral load which can keep a patient from moving into the third stage of HIV infection, AIDS, and can reduce the risk of a patient infecting their partner.7
PrEP Facts and Provider Awareness
PrEP Facts
PrEP is an underused tool in primary care11
Many practitioners will not provide prescriptions to those with the highest risk due to misconceptions about the harm reduction model6. Clinical studies DO NOT support this concern2
PrEP is a once a day pill that reduces the risk of acquiring HIV by move that 90%12
Information to consider
In 2010 the National HIV/AIDS Strategy (NHAS) was developed in order to give the United States goals to reach in regards to HIV and AIDS care and infection prevention11.
Primary Goals11
- Decrease the number of new HIV infections
- Improve quality of care for those living with HIV
- Decrease Health disparities in treating individuals with HIV
- Develop a nationwide response to the HIV epidemic11
According to the Body of literature gaps in care are caused by two factors11
- Poor engagement in care
- Low retention rates in care11
Many academic programs for health care professionals are beginning to recognize this gap and are responding by teaching about disparities in care that effects vulnerable populations11. While this is an amazing first step, there is a gap between the learned knowledge and students applying this knowledge. The literature identifies this as an area of development as Inter-professional trainings seems to be the starting point but the next step has not been identified11.
Barriers to Care
Many barriers to care are due to myths that surround medical care. The top four myths are the following6:
- PrEP Leads to higher risk behaviors6
- The literature does not support this concern
- Patients who engage in risk taking behaviors are less likely to be medically compliant6
- The literature shows that patients who are prescribed PrEP adhere to treatment in large numbers
- Remember that contemplation or pre-contemplation for one behavior change does not mean this is the same for other behavior changes
- There is a high risk of drug interactions6
- The alternative to side effects is new HIV infection
- Medical science considers PrEP to be a “safe and well tolerated medication”6
Other concerns
- Providers lack confidence in choosing who would be best served by taking PrEP6
- Training can help improve confidence
- Cost
- Even though the out of pocket cost can be high, most insurances and Medicaid provide coverage
- The manufacturer also has a medication assistance program6
- Remember that PrEP is a part of a behavioral change not a stand-alone intervention6
- Patients should attend routine doctors’ appointments
- STI screening should occur regularly
- Patients should be linked to other support services if applicable
- Condoms should be offered6
- At Risk Populations
- Those most at risk for acquiring HIV are the most likely to have trouble accessing PrEP12
- Due to health insurance disparities
- Limited community awareness remains an issue
- Stigma and distrust of the medical community is a large barrier to care for at risks populations especially people of color12
- Those most at risk for acquiring HIV are the most likely to have trouble accessing PrEP12
References
- About HIV/AIDS. (2018, July 23). Retrieved from https://www.cdc.gov/hiv/basics/whatishiv.htm
- About HIV/AIDS:PrEP. (2018, July 23). Retrieved from https://www.cdc.gov/hiv/basics/whatishiv.html
- About HIV/AIDS:PeP. (2018, May 23). Retrieved from https://www.cdc.gov/hiv/basics/whatishiv.html
- Centers for Disease Control and Prevention. HIV Surveillance Report, 2016; vol. 28. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published November 2017. Accessed November 29, 2017.
- Centers for Disease Control and Prevention. Estimated HIV incidence and prevalence in the United States, 2010-2015. HIV Surveillance Supplemental Report 2017;23(No. 1). http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published March 2018.
- Cotler, K., Yingling, C., & Broholm, C. (2018). Preventing new human immunodeficiency virus infections with pre-exposure prophylaxis. The Journal for Nurse Practitioners, 14(5), 376-382. doi:https://doi.org/10.1016/J.NURPRA.2017.12.021
- HIV Treatment. (2018, August 27). Retrieved from https://www.cdc.gov/hiv/basics/whatishiv.html
- HIV Treatment as Prevention. (2018, September 10). Retrieved from https://www.cdc.gov/hiv/risk/art/index.html
- Infectious diseases. (2018, January 03). Retrieved from https://www.mayoclinic.org/diseases-conditions/infectious-diseases/symptoms-causes/syc-20351173
- Maryland Annual HIV Epidemiological Profile 2016. Center for HIV Surveillance, Epidemiology and Evaluation, Maryland Department of Health, Baltimore, MD. 2017.
- Migano, J., Sofolahan-Oladeinde, Y., Hossain, M., Reitz, A., Polivka, J., Spencer, D., & Redfield, R. (2016). Preparing the future: An interprofessional approach to prepare future health and service-delivery professionals to attain an aids-free generation. Journal of Interprofessional Education and Practice, 4(1). doi:http://dx.doi.org/10.1016/j.xjep.2016.04.001
- Undetectable = Untransmittable: Introduction. (n.d.). Retrieved from https://www.preventionaccess.org/undetectable
- Goldstein, R. H., Streed, C. G., & Cahill, S. R. (2018). Being PrEPared — Preexposure Prophylaxis and HIV Disparities. New England Journal of Medicine, 379(14), 1293-1295. doi:10.1056/nejmp1804306